“My past is an armor I cannot take off, no matter how many times you tell me the war is over.”
Tomorrow I will walk through the doors of the Lurie Cancer Center as I have many times before. This routine has become all too familiar. Over nine months of treatment mixed with numerous other visits and hospitalizations allows me to walk the halls of Northwestern with ease and eerie familiarity.
It starts with a visit to port draw to get my blood drawn. This is hands down one the hardest part of the visit for me. Hours before my appointment I begin preparing for this by applying a numbing cream to my chest port—a small device surgically implanted into my chest that helps deliver medication and make for easier blood draws during treatment.
For many cancer patients, our port devices stay in long after our cancer treatment—sometimes for years because of the risk for potential relapse. Until then, it requires routine flushes by a medical professional. While showering or getting dressed, this protruding bump in my chest is a constant reminder of my treatment and the fact that my journey is far from over.
Next, I will wait to see my oncologist and get the results of my latest blood work. I will hold my breath as she palpates the lymph nodes in my neck, chest and lower body. I pray that I hear the words, “Everything looks good. See you in a few months.” Yet I also try to mentally prepare myself for the potential ‘what ifs’. Will I need another repeat scan? What if my blood work is off?
Many people believe that going into “remission” means victory—that one has defeated their disease and they have moved on to recovery. Surely, remission marks a major turn in cancer care, but it is more complicated than simply being done with cancer treatment.
The following is a vivid glimpse into the reality of being a cancer survivor.
Imagine you're going about your day, minding your own business, when someone sneaks up behind you...
You feel something press up against the back of your head, as someone whispers in your ear.
"Sssshhhhh.... don't turn around. Just listen. I am holding a gun against the back of your head. I'm going to keep it there. I'm going to follow you around like this every day, for the rest of your life."
"I'm going to press a bit harder, every so often, just to remind you I'm here, but you need to try your best to ignore me, to move on with your life. Act like I'm not here, but don't you ever forget... one day I may just pull the trigger... or maybe I won't. Isn't this going to be a fun game?"
This is what it is like to be diagnosed with cancer. Any STAGE of cancer. Any KIND of cancer. Remission does not change the constant fear. It never truly goes away. It's always in the back of your mind.
Please, if you have a loved one who has ever been diagnosed with cancer, remember this. They may never talk about it or they may talk about it often. Listen to them.
They aren't asking you to make it better. They want you to sit with them in their fear... their sadness... their anger... just for the moment. That's it.
Don't try to talk them out of how they are feeling. That doesn't help. It will only make them feel like what they are going through is being minimized. Don't remind them of all the good things they still have in their life. They know. They are grateful.
But some days they are more aware of that gun pressing into the back of their head and they need to talk about it. Offer them an ear.Source: The Teal Society, @thewombtangclan
No Evidence of Disease, Lingering Trauma
“There is no timestamp on trauma. There isn’t a formula that you can insert yourself into to get from horror to healed. ”
In the US, 1 in 2 women and 1 in 3 men will develop cancer in their lifetime. It is often said there are four phases to dealing with cancer; diagnosis, waiting for test results, treatment and the period following treatment or remission.
Thanks to advances in treatment and early detection, more people than ever are becoming cancer survivors. As survivors, it’s often understood but less often spoken about that the assault to our bodies and minds as cancer patients extends far beyond our last treatment cycle.
Remission itself brings reassurance and a sense that period of calm and recovery is now within reach. You have been given a second chance to rewrite the rules and try living differently with greater appreciation. In truth, remission does NOT mean you are all clear. Instead, remission the hope that your active cancer treatment is about to be a closed chapter in your life. It means finding a way to move forward while still under routine monitoring for potential relapse.
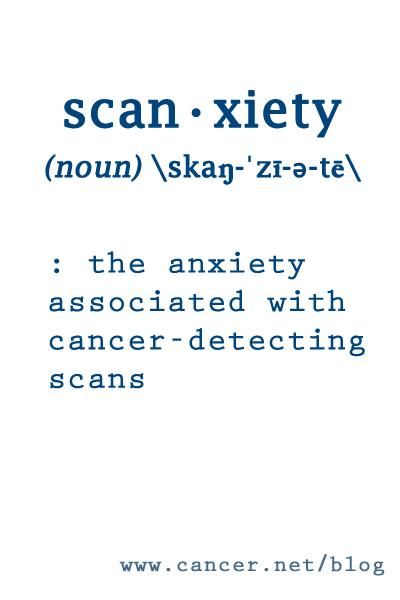
Life goes on and relief flourishes after you are told you are in remission. Then, a few months go by and the next appointment looms on the horizon. The cycle of dread and worry repeats. This cycle repeats over and over for the first few months and sometimes up to five years or more after you are diagnosed.
I’ve learned part of living in remission is learning to manage the fluid emotions of joy and gratitude intermixed with the feelings of guilt, shame, anger and fear. Post-cancer life is often interwoven with moments of empowerment followed by a somber reckoning that this way of life has become your “new normal.” There are periods of immense joy and elation that come with the news you are “in remission.” Then there are long periods of waiting and worrying if the next visit to the doctor will bring more freedom or news of a potential relapse. There are countless daily reminders of what you have been through and the reality of what could be around-the-corner.
Guilt
At times, I’ll be the first to admit I often feel a sense of guilt when it comes from my cancer treatment. Guilty for being able to receive one of the latest advancements in cancer treatment (immunotherapy) and surviving when so many others who were diagnosed after me, some younger than I, have since died. Guilty for going on about my cancer journey long after my treatment has finished. Guilty for not always remembering to be thankful and seize the day. And guilty for all the trouble and worry I put my loved ones through.
Anger
Some people (myself included) become angry after treatment. Some struggle to get past the trauma, while others learn from it and use it as a catalyst to live life in a completely different way. Any traumatic life event that you go through will leave scars and people survive in different ways. Chemo and radiation save our lives, but they also cause a hell of a lot of side effects, including secondary cancers and painful, lingering side effects like neuropathy and gastrointestinal issues.
Feeling Broken
For most cancer survivors, the first year in remission is often the most difficult This is because when you’re in remission, it finally hits you that you literally almost died and spent the majority of the last year fighting for your life. It’s a startling realization to take in and fully process. When you’re going through treatment, you’re in survival mode—too sick and tired to actually realize what’s really going on. Remission lends the opportunity to reflect on the good and the bad. Getting diagnosed and treated for cancer can leave you at times feeling broken, helpless and largely distrusting of your body. In my experience, remission at first turned my survival mode into a state of hyper-vigilance where any unusual symptom made me flip out and almost convinced I was in the throes of a possible relapse.
Cancer survivors are tasked with carrying on with their lives by learning to adapt to a “new normal” that comes with being in remission. We must rediscover who we truly are under all the layers of trauma our cancer treatment may have caused. We must learn to find our footing and move forward amidst the shifting sands of fearlessness and fear, confidence and worry, relief and calm, certainty and uncertainty. Our sense of cautious optimism grows with each disclosure that our cancer has not spread and there is no evidence of disease. Over time, we learn to breathe a little easier, while the fear is always there—it seems to move further and further to the back of our minds.
Addressing and understanding the emotions you are experiencing as a result of cancer or any disease is difficult. It’s painful. But I’ve come to learn and accept it’s entirely necessary to heal. Seeking out community—a therapist, friend or family member, or a support group of others who have experienced similar trauma like cancer—is a crucial step in recovery. I’m hopeful that in time I will be able to transform this horrible, traumatic experience from an endless stressor into a source of strength.
Overcoming Fear with Gratitude
One way I am trying to overcome my anxiety and lingering fear regarding my treatment is by expressing daily gratitude. The latest research in neuroscience shows that when we practice gratitude we are actively rewiring our brains and naturally boosting our serotonin levels. According to neuroscientist Dr. Alex Korb, all we need to do is simply ask, “What am I grateful for?” No answers are necessary. Just searching helps.
Some ways to practice gratitude:
Keep a gratitude journal.
Tell a loved one or a friend something you appreciate about them.
Look at yourself in the mirror and think of something you like about yourself.
Sit in a quiet place and think about when something went well. How did that feel? Practice that feeling every day for a week.
Next time something bad happens consider 5 good things that happened as a result of this event.
Write someone a thank you note.
Write it down, talk about it, think about it, re-live it, meditate.
It has been said that trauma creates change you don’t choose; whereas healing creates change you do choose. There is a great transition from patient to survivor. I believe the journey from patient to survivor begins with patience. We must be patient with ourselves and give our bodies and minds time to heal from all the trauma we have endured. Healing comes moment by moment and one breath at a time.
Sources:
Cancer Truths- The Teal Society
'1 in 2 people will develop cancer in their lifetime'- Medical News Today, 2015
The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a Time by Alex Korb, PhD